Healthcare Claims Management Market | Acumen Research and Consulting
Healthcare Claims Management Market Size - Global Industry, Share, Analysis, Trends and Forecast 2024 - 2032
Published :
Report ID:
Pages :
Format :
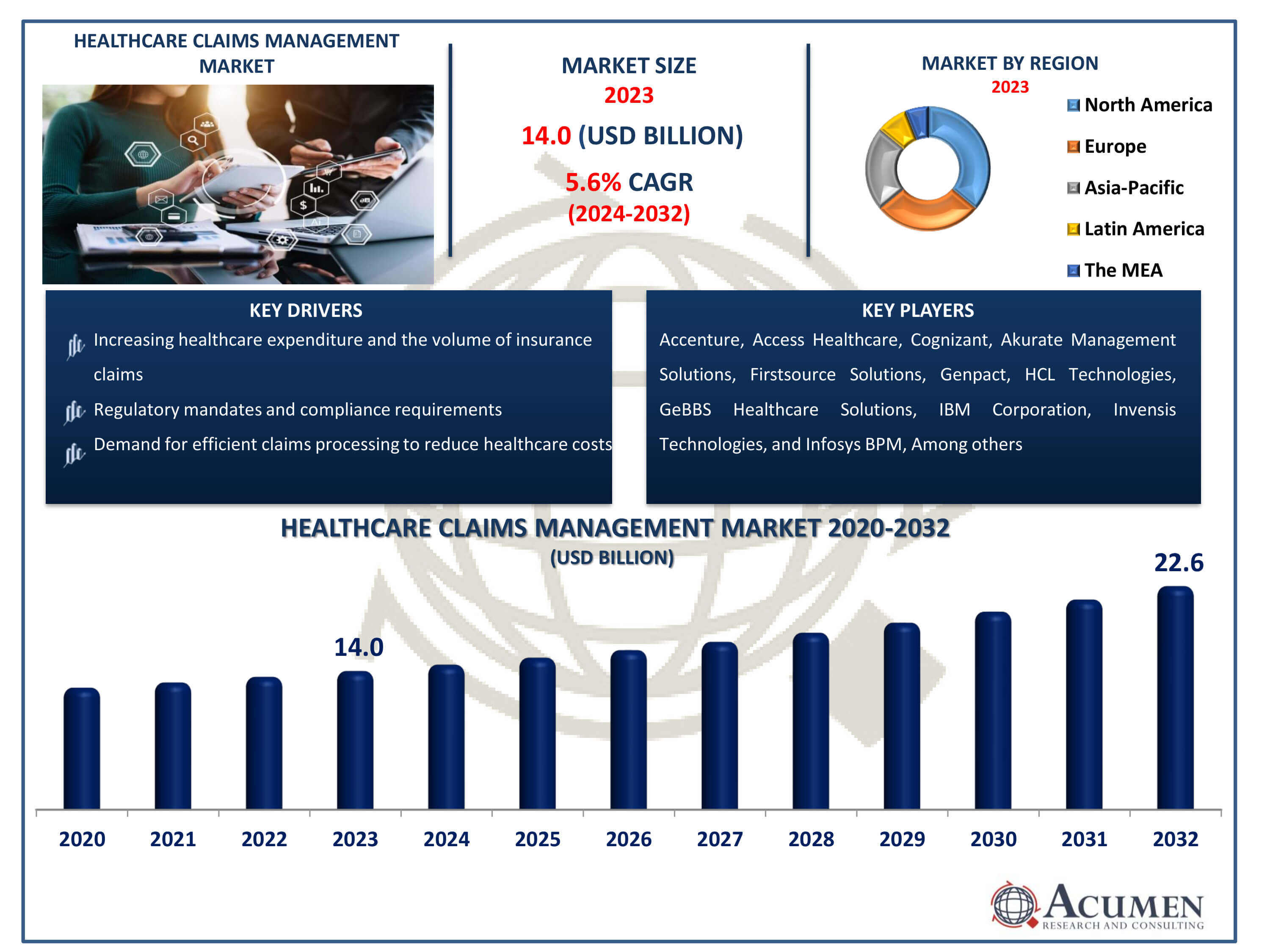
The Healthcare Claims Management Market Size accounted for USD 14 Billion in 2023 and is estimated to achieve a market size of USD 22.6 Billion by 2032 growing at a CAGR of 5.6% from 2024 to 2032.
Healthcare Claims Management Market Highlights
- Global healthcare claims management market revenue is poised to garner USD 22.6 billion by 2032 with a CAGR of 5.6% from 2024 to 2032
- North America healthcare claims management market value occupied around USD 5.04 billion in 2023
- Asia-Pacific healthcare claims management market growth will record a CAGR of more than 6% from 2024 to 2032
- Among type, the integrated solutions sub-segment generated over 70% share in 2023
- Based on end-use, the healthcare provider sub-segment generated around 65% share in 2023
- Entry into emerging markets with evolving healthcare systems is a popular healthcare claims management market trend that fuels the industry demand
The healthcare claims management industry is the economic sector in which health insurance claims are filed, monitored, and administered. It consists of a multitude of software programs and services aimed at simplifying the onerous and time-consuming process of filing, processing, and settling medical claims. This market is critical to the healthcare ecosystem because it assures accurate and fast claims processing, reduces fraud, and improves payer and provider financial performance. The Healthcare Claims Management Market is continually changing due to the ongoing digital transformation and the growing importance of healthcare cost control.
Global Healthcare Claims Management Market Dynamics
Market Drivers
- Increasing healthcare expenditure and the volume of insurance claims
- Growing adoption of electronic health records (EHR) and digital health systems
- Regulatory mandates and compliance requirements
- Demand for efficient claims processing to reduce healthcare costs
Market Restraints
- Complex and evolving healthcare regulations
- Data security and privacy concerns
- Resistance to technology adoption in some healthcare organizations
Market Opportunities
- Advancements in artificial intelligence and machine learning for claims processing
- Expansion of telehealth services and remote patient monitoring
- Demand for cloud-based claims management solutions
Healthcare Claims Management Market Report Coverage
| Market | Healthcare Claims Management Market |
| Healthcare Claims Management Market Size 2022 | USD 14 Billion |
| Healthcare Claims Management Market Forecast 2032 | USD 22.6 Billion |
| Healthcare Claims Management Market CAGR During 2023 - 2032 | 5.6% |
| Healthcare Claims Management Market Analysis Period | 2020 - 2032 |
| Healthcare Claims Management Market Base Year |
2022 |
| Healthcare Claims Management Market Forecast Data | 2023 - 2032 |
| Segments Covered | By Type, By Component, By Deployment Mode, By End-Use, And By Geography |
| Regional Scope | North America, Europe, Asia Pacific, Latin America, and Middle East & Africa |
| Key Companies Profiled | eClinicalWorks LLC, Optum, Inc,, Allscripts Healthcare Solutions, Inc., The SSI Groups Inc., COGNIZANT TECHNOLOGY SOLUTIONS CORPORATION, Oracle Corporation, McKesson Corporation, GE Healthcare, Quest Diagnostics, Athenahealth Inc. |
| Report Coverage |
Market Trends, Drivers, Restraints, Competitive Analysis, Player Profiling, Covid-19 Analysis, Regulation Analysis |
Healthcare Claims Management Market Insights
The growing number of patients with chronic diseases and the increase in healthcare claims has fueled the demand for healthcare claims management solutions. According to the National Association of Insurance Commissioners (NAIC), the direct written premiums for the accident and health insurance industry reached $1.1 trillion in 2018, a significant 57.3% increase from 2009. The ten largest insurers accounted for 51.8% of the total U.S. market. As healthcare costs continue to rise annually, more consumers are opting for health insurance. Enhanced insurance policies provided by the government are making this a more attractive and secure option for consumers.
According to the Congressional Research Service, approximately 58 million people (18.1% of the U.S. population) were enrolled in Medicare in 2019, boosting the need for efficient claims management solutions. Leading industry players are concentrating on expanding their operations through strategic acquisitions, aiming to grow their customer base and boost revenue. This trend is anticipated to drive the growth of the healthcare claims management market.
The introduction of innovative solutions to expand product portfolios is anticipated to drive the growth of the healthcare claims management market. However, several challenges could impede this growth, including the high costs associated with product development and deployment, as well as concerns about data security. Additionally, a shortage of skilled professionals is expected to hinder market expansion. Despite these obstacles, the increasing adoption of cloud technology and the integration of AI in healthcare present new opportunities for market participants. Furthermore, the rising number of insurance cases and a focus on exploring untapped markets in developing countries are projected to boost revenue generation in the healthcare claims management market. According to the Current Population Survey Annual Social and Economic Supplement, a significant percentage of people lacked health insurance at some point during the year.
Healthcare Claims Management Market Segmentation
The worldwide market for healthcare claims management is split based on type, component, deployment mode, end-use, and geography.
Healthcare Claims Management Type
- Integrated Solutions
- Standalone Solutions
Integrated solutions dominate the healthcare claims management industry, with market forecasts supporting this trend. These solutions offer a comprehensive approach to claims processing, seamlessly integrating all stages from submission to reimbursement. They enhance efficiency, reduce errors, and ensure data accuracy, resulting in faster claims adjudication. Integrated solutions also facilitate compliance with stringent regulatory requirements, a crucial aspect of the healthcare industry.
Furthermore, market forecasts indicate sustained growth in the demand for end-to-end automation and interoperability in healthcare claims administration, aligning with the broader trend of digital transformation in healthcare. Consequently, integrated solutions are well-positioned to maintain their market dominance, providing healthcare providers and payers with a pathway to enhanced efficiency and compliance.
Healthcare Claims Management Component
- Software
- Services
Software is the cornerstone of the healthcare claims management industry, with market analysis affirming its dominant role. It is crucial for automating and streamlining the intricate claims processing workflow, making it the largest segment in the market. Healthcare organizations depend on robust software solutions to efficiently handle the complex administrative and financial tasks involved in claims management. These platforms significantly reduce manual labor and errors through features such as claims tracking, validation, and adjudication. Real-time data insights and analytics facilitate better decision-making. Software solutions align with the industry's focus on efficiency and digitization, reflecting the increasing demand for technologically advanced tools that enhance the speed and accuracy of claims processing.
Healthcare Claims Management Deployment Mode
- On-premise
- Cloud-based
- Web-based
The web-based segment of the healthcare claims management market is the largest due to its flexibility and accessibility. Web-based solutions are highly convenient for healthcare providers, payers, and administrators because they can be accessed from any device with an internet connection. These solutions reduce the need for software installations and updates and eliminate the necessity for complex on-premise infrastructure. The adaptability and ease of access of web-based solutions make them the preferred choice for many healthcare organizations, contributing to their market dominance.
Healthcare Claims Management End-Use
- Healthcare Payers
- Healthcare Provider
- Other
In the healthcare claims management market, the web-based category holds the largest share, driven by a strategic shift towards cloud-based solutions for enhanced claims processing efficiency. The healthcare industry increasingly adopts web-based solutions for claims administration due to their cost-effectiveness and scalability. Market analysis indicates that healthcare payers and providers benefit from easy, remote access to claims data, enabling rapid decision-making and improved operational efficiency. This trend aligns with the broader market movement towards cloud-based solutions, establishing web-based platforms as the industry standard for healthcare claims management.
Healthcare Claims Management Market Regional Outlook
North America
- U.S.
- Canada
Europe
- U.K.
- Germany
- France
- Spain
- Rest of Europe
Asia-Pacific
- India
- Japan
- China
- Australia
- South Korea
- Rest of Asia-Pacific
Latin America
- Brazil
- Mexico
- Rest of Latin America
The Middle East & Africa
- South Africa
- GCC Countries
- Rest of the Middle East & Africa (ME&A)

Healthcare Claims Management Market Regional Analysis
North America stands as the largest regional player in the healthcare claims management market, a significance attributed to several key factors. Primarily, its well-established and well-funded healthcare infrastructure has positioned North America as an early adopter of advanced healthcare technologies, including claims management systems. Additionally, the region's complex and heavily regulated healthcare system necessitates effective claims administration, making the adoption of advanced technologies crucial. For instance, in October 2023, Optum completed their merger with Change Healthcare. The companies unifying goal is to build a simpler, more intelligent and adaptable health-care system for patients, payers, and providers. The sheer scale of the North American healthcare market, encompassing numerous insurance companies and healthcare facilities, drives the high demand for robust claims management systems. Market forecasts further affirm North America's leadership in the healthcare claims management market.
The Asia-Pacific region is experiencing the fastest growth in the healthcare claims management industry. This rapid expansion can be attributed to the developing healthcare sector, bolstered by a growing middle class, increased access to healthcare, and a rising number of healthcare providers. For instance, in April 2023, Welldoc and Conifer Health Solutions announced a collaboration to launch Conifer Connect, a tailored digital health app designed to assist members in managing their daily health while developing relationships with their personal health nurse. As healthcare becomes more complex, there is a growing need for specialized claims management solutions. Additionally, Asia-Pacific is a preferred hub for business process outsourcing (BPO) services, due to its highly skilled workforce and cost-effective labor markets. The demand for claims management services in the region is further driven by the adoption of innovative technology and digital healthcare solutions. With its dynamic environment, embrace of outsourcing, and use of new technologies, Asia-Pacific has emerged as the fastest-growing player in the global healthcare claims management market.
Healthcare Claims Management Market Players
Some of the top healthcare claims management companies offered in our report includes eClinicalWorks LLC, Optum, Inc,, Allscripts Healthcare Solutions, Inc., The SSI Groups Inc., COGNIZANT TECHNOLOGY SOLUTIONS CORPORATION, Oracle Corporation, McKesson Corporation, GE Healthcare, Quest Diagnostics, and athenahealth Inc.
- In 2021, Majesco, a global provider of cloud insurance platform software, acquired ClaimVantage. This acquisition is expected to enable the company to offer next-generation insurance technology solutions, allowing insurers to accelerate their digital transformation to meet the demands of tomorrow. It is anticipated that this move will expand the company's product offerings and enhance its overall business.
- In 2020, Change Healthcare, a global healthcare technology company, acquired the 'PROMETHEUS Analytics' solution from Altarum. This product acquisition is expected to enhance the company's business and increase its revenue share in the global market.
Frequently Asked Questions
How big is the healthcare claims management market?
The healthcare claims management market size was USD 14 Billion in 2023.
What is the CAGR of the global healthcare claims management market from 2024 to 2032?
The CAGR of healthcare claims management is 5.6% during the analysis period of 2024 to 2032.
Which are the key players in the healthcare claims management market?
The key players operating in the global market are including eClinicalWorks LLC, Optum, Inc,, Allscripts Healthcare Solutions, Inc., The SSI Groups Inc., COGNIZANT TECHNOLOGY SOLUTIONS CORPORATION, Oracle Corporation, McKesson Corporation, GE Healthcare, Quest Diagnostics, and athenahealth Inc.
Which region dominated the global healthcare claims management market share?
North America held the dominating position in healthcare claims management industry during the analysis period of 2024 to 2032.
Which region registered fastest CAGR from 2024 to 2032?
Asia-Pacific region exhibited fastest growing CAGR for market of healthcare claims management during the analysis period of 2024 to 2032.
What are the current trends and dynamics in the global healthcare claims management industry?
The current trends and dynamics in the healthcare claims management industry include increasing healthcare expenditure and the volume of insurance claims, growing adoption of electronic health records (EHR) and digital health systems, regulatory mandates and compliance requirements, and demand for efficient claims processing to reduce healthcare costs.
Which type held the maximum share in 2023?
The integrated solutions type held the maximum share of the healthcare claims management industry.