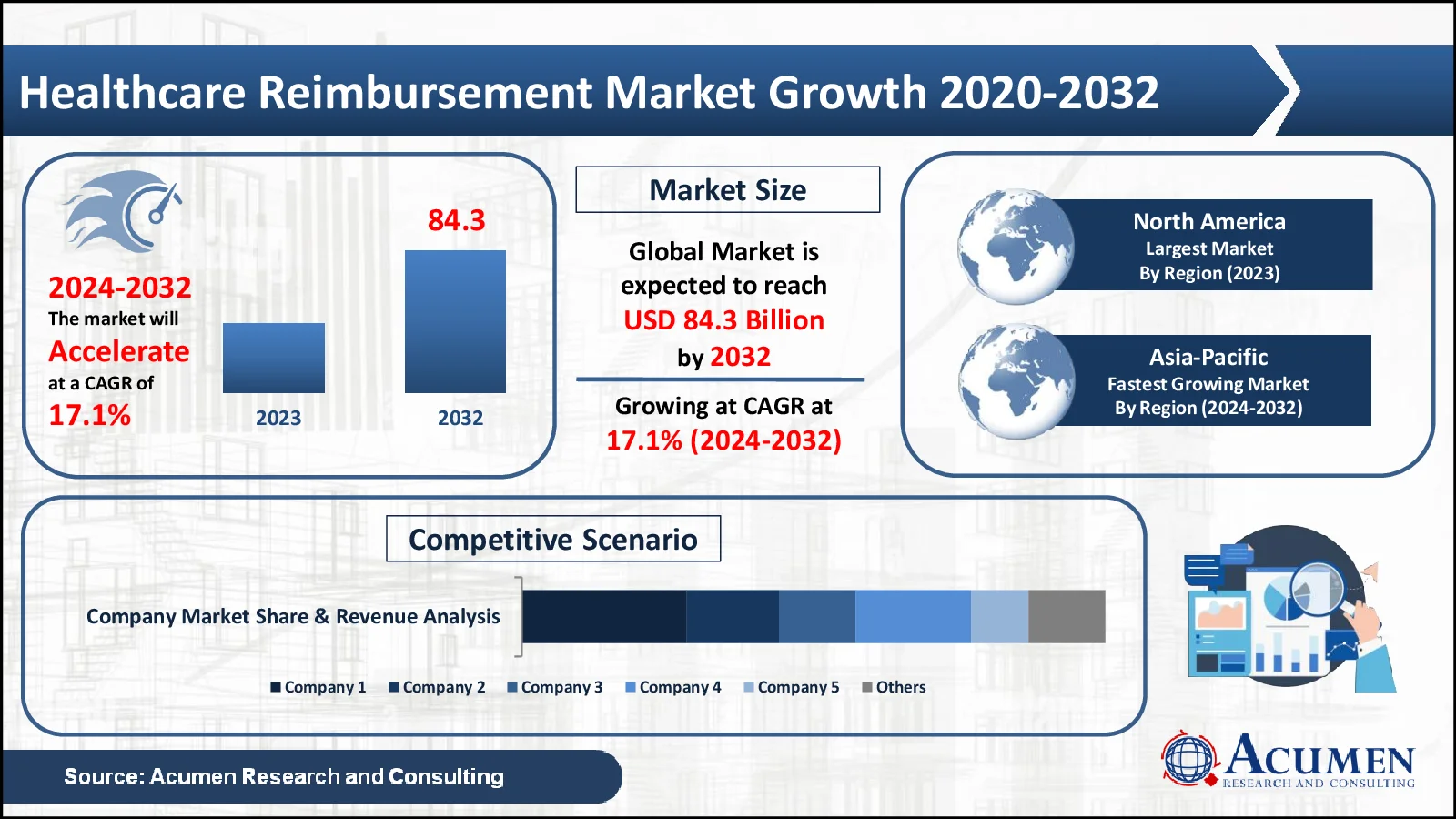
Healthcare Reimbursement Market Size to Reach USD 84.3 Billion by 2032 growing at 17.1% CAGR - Exclusive Report by Acumen Research and Consulting
The Healthcare Reimbursement Market, valued at USD 21.2 Billion in 2023, is anticipated to surpass USD 84.3 Billion by 2032, reflecting a projected CAGR of 17.1%
The healthcare reimbursement market is a pivotal component of the healthcare industry, encompassing the mechanisms and processes by which healthcare providers receive payment for their services from insurance companies and government programs. This market is driven by the need for efficient and transparent payment systems that ensure timely and accurate compensation for medical services rendered. Key drivers of the healthcare reimbursement market include the increasing prevalence of chronic diseases, the aging population, and the expansion of health insurance coverage. The rising incidence of chronic conditions such as diabetes, cardiovascular diseases, and cancer necessitates frequent medical interventions, thereby boosting the demand for efficient reimbursement systems. Additionally, government initiatives to provide healthcare access to a broader population base, coupled with the implementation of health insurance mandates, have significantly increased the number of insured individuals, further propelling market growth.
Technological advancements in healthcare IT systems, including electronic health records (EHR) and healthcare claims management software, are transforming the reimbursement landscape. These technologies facilitate the automation of billing processes, reduce administrative errors, and enhance the speed and accuracy of claim submissions and approvals. The integration of artificial intelligence (AI) and machine learning (ML) in these systems is also expected to improve fraud detection and streamline the reimbursement process. Despite the positive outlook, the market faces several challenges, including regulatory complexities and the varying reimbursement policies across different regions. The administrative burden associated with managing and processing claims, as well as the potential for claim denials and delays, poses significant hurdles for healthcare providers.
Healthcare Reimbursement Market Statistics
- In 2023, the global healthcare reimbursement market was valued at USD 21.2 billion
- The market is anticipated to grow at a consistent annual rate of 17.1% from 2024 to 2032
- North America dominates the market, accounting for 41% of the total share
- The Asia-Pacific region is expanding rapidly, with an impressive annual growth rate of 18%
- The private payers sector was the largest revenue generator in 2023
- There has been a significant increase in revenue growth within the hospital service provider segment
- A key emerging trend is the expansion of value-based care models
Access Table Of Content: https://www.acumenresearchandconsulting.com/table-of-content/healthcare-reimbursement-market
Healthcare Reimbursement Market Dynamics
Increasing Prevalence of Chronic Diseases Fuels the Healthcare Reimbursement Market
The primary driver of the healthcare reimbursement market is the escalating prevalence of chronic diseases. Chronic conditions such as diabetes, cardiovascular diseases, cancer, and respiratory disorders have been rising globally, largely due to factors like aging populations, sedentary lifestyles, and unhealthy diets. These conditions often require ongoing medical attention, frequent hospital visits, long-term treatment plans, and continuous medication, all of which generate a substantial volume of healthcare services that necessitate efficient reimbursement systems.
Healthcare providers need reliable reimbursement mechanisms to manage the financial aspects of treating chronic diseases effectively. The increasing number of patients with chronic illnesses puts pressure on healthcare systems to deliver timely and high-quality care, which in turn demands streamlined and transparent reimbursement processes. Insurance companies and government programs are pivotal in covering the costs associated with chronic disease management, including consultations, diagnostic tests, medications, and hospitalizations.
Moreover, as governments and health organizations emphasize preventive care and early intervention, the demand for services related to chronic disease management continues to surge. This trend not only amplifies the need for robust reimbursement systems but also drives innovation in health insurance policies and reimbursement models to accommodate the growing patient base and the complexity of chronic care.
Integration of Artificial Intelligence in Reimbursement Processes Offers Significant Healthcare Reimbursement Market Opportunities
An exciting opportunity within the healthcare reimbursement market lies in the integration of artificial intelligence (AI) into reimbursement processes. AI technologies have the potential to revolutionize the way healthcare claims are managed, processed, and analyzed, offering significant benefits for both healthcare providers and payers. Advantages of AI integration are the enhancement of accuracy and efficiency in claims processing. AI algorithms can quickly analyze vast amounts of data, identifying patterns and anomalies that might indicate errors or fraudulent claims. This capability reduces the administrative burden on healthcare providers and insurers, minimizes the risk of claim denials, and speeds up the reimbursement process, ensuring that providers receive timely payments for their services.
Furthermore, AI-driven predictive analytics can offer valuable insights into claim trends and patient outcomes, helping insurers develop more precise and fair reimbursement policies. By leveraging AI, insurers can predict which claims are most likely to be approved, optimize reimbursement rates, and identify opportunities for cost savings. For healthcare providers, AI can streamline the documentation and coding processes, reducing the likelihood of human error and ensuring that claims are submitted accurately and promptly. In addition to improving operational efficiency, AI can enhance the patient experience by enabling faster and more transparent reimbursement processes. Patients can benefit from quicker resolution of claims and reduced out-of-pocket expenses, fostering greater trust in the healthcare system.
Healthcare Reimbursement Market Segmentation
The global market for healthcare reimbursement is classified into 4 groups: claim, payers, service provider, and regional markets
- Claim: underpaid, and full paid
- Payers: private payers, and public payers
- Service provider: physician office, hospitals, diagnostic laboratories, and others
- Regional: Latin America, North America, Asia-Pacific, the Middle East & Africa, and Europe
Healthcare Reimbursement Market Regional Outlook
North America dominates the healthcare reimbursement market, primarily due to the well-established healthcare infrastructure and the presence of major market players. Europe and the Asia-Pacific regions are also witnessing substantial growth, driven by increasing healthcare expenditures and government efforts to expand healthcare access.
Healthcare Reimbursement Market Players
Healthcare reimbursement companies profiled in the report include Allianz Group, Aviva, Agile Health Insurance, BNP Paribas, The Blue Cross Blue Shield Association, Nippon Life Insurance, Aetna, UnitedHealth Group, CVS Health, and Wellcare Health Plans.
Enquire Before Buying https://www.acumenresearchandconsulting.com/inquiry-before-buying/1004
Receive our personalized services and customization by clicking here https://www.acumenresearchandconsulting.com/request-customization/1004
Mr. Richard Johnson
Acumen Research and Consulting
India: +91 8983225533


